Summary
BACKGROUNDThe past 25 years have seen the increased use of minimally invasive surgery. The development of these techniques has impacted the domain of liver surgery. This study aimed to describe the safety, feasibility, benefits and results of laparoscopic liver resection in a single tertiary care centre.
METHODS
We reviewed the medical records of all patients who underwent liver surgery between January 2005 and December 2016 at the University Hospital of Basel. We selected all liver resections performed by laparoscopic surgery. To evaluate the results of the laparoscopic liver surgery, we chose the following data: the conversion rate from laparoscopy to open surgery, the median operating time, postoperative complications, the median length of stay following surgery and the median surgical margin in patients with malignant lesions.
RESULTS
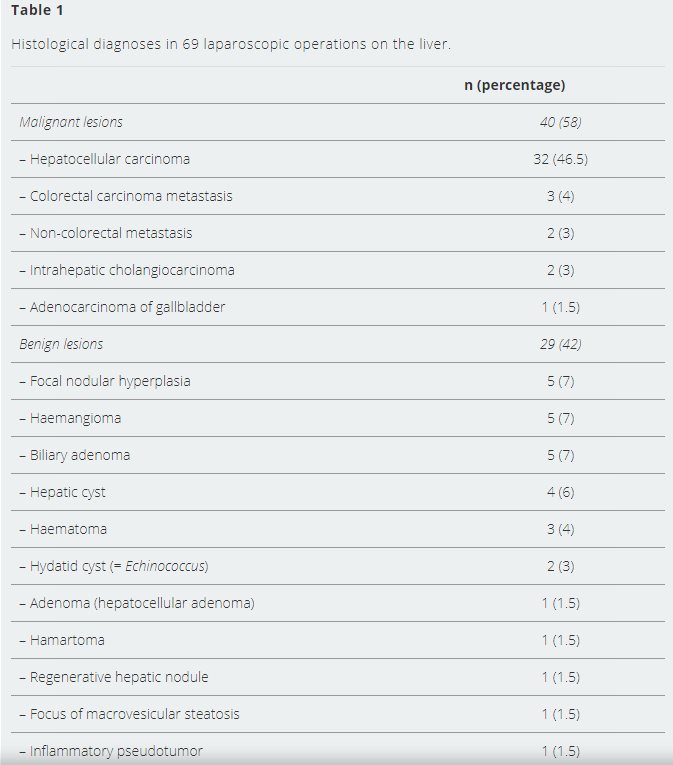
Of the 274 liver operations, 201 (73%) were performed by open surgery and 73 (27%) by laparoscopy. Sixty-nine laparoscopic liver resections were included in this study. The selected laparoscopic liver resections were performed in 65 patients: 38 men and 27 women. The median age was 59 (range 29–85) years. Forty resections were performed for malignant lesions and 29 (42%) for benign diseases. The median operating time was 112 (range 50–247) minutes. The conversion rate was 19%. The most common cause for conversion was bleeding (69% of all conversions, 13% of all patients). Postoperative complications occurred in 15 patients (22%). The median hospitalisation time was 7.1 (range 2–23) days. Thirty-two patients (46.5% of all patients) had hepatocellular carcinoma. The mean tumour size was 25.6 (range 5–55) mm. The median surgical margin was 9 mm.
CONCLUSION
This study showed that in our centre laparoscopic liver surgery is a safe and effective treatment option for both benign and malignant liver lesions.
Keywords: laparoscopic liver resection, laparoscopic hepatectomy, hepatocellular carcinoma, HCC
Introduction
Minimally invasive liver resections are less invasive because they avoid large laparotomy wounds. These techniques allow a local or closed surgery and are characterised by many advantages, such as less abdominal wall morbidity, better cosmetic outcome and faster recovery [1].Although the first laparoscopic liver resection was reported in the early 1990s, minimally invasive liver surgery came up against several barriers to widespread use. These obstacles included fear of uncontrollable haemorrhage, difficulty of performing an operation with the laparoscopic technique, difficulty of reproducing mobilisation and operative conditions used in open surgery, the longer learning process needed to obtain familiarity with laparoscopy and concerns about the oncological outcomes [2–4].
Nevertheless, in the last two decades laparoscopic liver resection has developed dramatically. As Nguyen et al. report in their global review of nearly 3000 laparoscopic liver resections, this surgical procedure has evolved dramatically, with improved understanding of the anatomical segments of the liver, enhanced imaging by computed tomography and magnetic resonance imaging scans, improved anaesthesia, critical care and postoperative nursing and technological advances in laparoscopic devices [2, 5].
Initially, most authors considered laparoscopic liver resection suitable only for benign lesions and for minor or wedge resections. However, in recent years, laparoscopic resection has been extended to more complex interventions such as major liver resection and malignant lesions [4, 6–8].
This study aimed to describe the experience and the results of laparoscopic liver resection at a single centre over 12 years.
Patients and methods
The medical records of all patients who underwent liver operations between January 2005 and December 2016 at the University Hospital of Basel were reviewed retrospectively.Cases were identified with a keyword search of our electronic health records.
All surgical procedures intended to perform any operation other than liver resection were excluded from the study.
From the 274 liver interventions selected, we chose those operations performed by minimally invasive (laparoscopic) surgery. Cases converted to open surgery were included in the study and constitute the conversion rate from laparoscopic to open surgery.
At our institution, three surgeons operate together to perform this type of surgery.
The operations included in the study were performed by a total of 15 different lead surgeons. Among these, three performed more than five operations as lead surgeon. Seven other surgeons were first assistant for more than five procedures.
Laparoscopic resection was performed under carbon dioxide pneumoperitoneum, with an intra-abdominal pressure of between 12 and 16 mm Hg. Four to six ports and a 30-degree laparoscope were generally used. Ultrasonographic exploration of the liver was performed before resection. An ultrasonic dissector (Thunderbeat; Olympus) or a harmonic scalpel (Ultracision; Ethicon) were used for parenchymal transection. Portal pedicles were sealed with clips or staplers and hepatic veins were divided using a linear stapler. Coagulation was performed with bipolar coagulation and an argon beamer. The resected liver specimen was extracted using an endobag, either through the umbilical access of the laparoscope or along a suprapubic horizontal incision. Abdominal drainage was usually omitted.
We present the following data: the conversion rate from laparoscopy to open surgery, the duration of the surgical operation, the postoperative complications, the hospital length of stay after the operation and the mean surgical margin for malignant lesions.
Patients’ baseline data, including demographics (age at time of surgery, patient’s sex), lesion pathology, location of lesions and extent of liver resection, were also extracted from the medical records and are presented in the results.
The Ethics Committee of Northwest and Central Switzerland evaluated our study and concluded that it fulfils the ethical and scientific standards for research according to the Human Research Act.
Results
Between January 2005 and December 2016, 274 liver operations were performed at the University Hospital of Basel: 201 operations were performed by open surgery (73%) and 73 by laparoscopy (27%).The 73 laparoscopic liver surgeries included 69 liver resections, one biopsy, one diagnostic laparoscopy and two diagnostic laparoscopies with biopsy.
The selected 69 laparoscopic liver resections were performed in 65 patients (38 men and 27 women) with a median age of 59 (range 29-85) years. Four patients were operated on twice during the study period.
Forty resections (58% of the 69 cases) were performed for malignant lesions and 29 (42%) for benign diseases (table 1).
==========
SOURCE*
